Maricopa County’s mental health terrain is littered with tracks that often do not meet at the ends, leaving people to essentially jump the tracks in attempt to land themselves at the necessary hubs or stations seeking the much needed services that contribute to overall mental health stabilization and well-being. The terrain of mental health services within Maricopa County includes a complex web of public and private entities offering services to multiple special population groups. The web of services is more like disconnected locations on a geo-spatial map than an interconnected network of care. This blog post focuses on the portion of the web of services that constitute the publicly funded mental health system of Maricopa County.
Maricopa’s publicly funded mental health system on the broadest level is comprised of EMS (911), police, fire, hospital ED, department of corrections, inpatient and community mental health care administered through contracts with Arizona State appointed Regional Behavioral Health Authority (RHBA), Mercy Care (via Arizona Health Care Cost Containment System (AHCCCS)). Each of these providers of care represent points along the terrain of local services. Each one of these large, complex service entities have operating policies that are mission guided and often influenced by interests of liability avoidance and cost efficiency factors. Additionally, with regard to the topic of mental health, only one of the public agencies listed, (Mercy Care), has a mission dedicated to serving the needs of people living with mental illness in our community. The other nodes in the publicly funded “system” of mental health care have a divided focus and mission. Emergency medical service provider systems (911, police, fire and hospital emergency departments) have missions aimed at saving human lives when acute physical trauma has been experienced. The nexus between the nodes in this system for acute physical injury have strong connections, at least in terms of design. The ties between the nodes in that system have clear alignment in terms of policies that facilitate the flow of critical interagency actions such as communication, transfer of care, and follow-up/preventative services.
The Department of Corrections (DOC) seems like an unlikely node in a system aimed at mental health and wellness because their mission is to serve and protect the people of Arizona by securely incarcerating convicted felons, by providing structured programming designed to support inmate accountability and successful community reintegration, and by providing effective supervision for those offenders conditionally released from prison. Their policies and network of interaction between police, jail, prison and probation are designed to facilitate an integrated system of interagency communication, collaboration, transfer of care and follow-up/preventative services.
Finally, the system dedicated to providing comprehensive public mental health services in Maricopa County is Mercy Care (AHCCCS) and its network of mental health care provider community clinics, hospitals and assertive community treatment (ACT) teams. The publicly funded mental health system is connected in terms of policy designed to align continuum of care, interagency collaboration, transfer of care and follow-up services. However, it is very difficult to connect the driving force behind policy design as being the improving patient outcomes when the name of agency empowered to design organizational operations through policy development is, Arizona Health Care Cost Containment System. The title highlights a driving mission focus, cost containment.
Arizona is underfunded when it comes to developing and providing a comprehensive mental health care system. Because of the lack of funding for a comprehensive system, there remains a scarcity of services, leaving people needing care, undertreated. The long term effects of lacking mental health treatment services are seen when mental illness further deteriorates into an unstable crisis state which all too often results in lost employment, housing, and/or incarceration.
Unfortunately all of these nodes comprise the Maricopa County mental health “system”. The navigation terrain is brindled in an array of disconnected mental health care access points most of which are undedicated to the care mission of providing mental health services. This lack of undedicated services leaves people in our community struggling to access mental health care by whatever means are most accessible. This is seen in the high utilization of the 911 system for non-emergent, mental health issues. It also means that EMS or DOC professionals trained to deliver services to a specific population are now fatigued by an ever widening “scope creep” as they becoming the new front line mental health professionals that they were never trained to be.
This train is running off the tracks. Tracing the tracks from the hub in the system the drivers of policy development become clear to this issue being a state funding and service alignment issue. The agency whose mission is to provide comprehensive mental health services to meet the needs of our population is not meeting the federal mandate. Using measures of rates homelessness, incarceration, and utilization of crisis nodes in the system it is clear to assess that Arizona is not yet meeting it fiduciary mandate set by our U.S. Mental Health Block Grant funding.
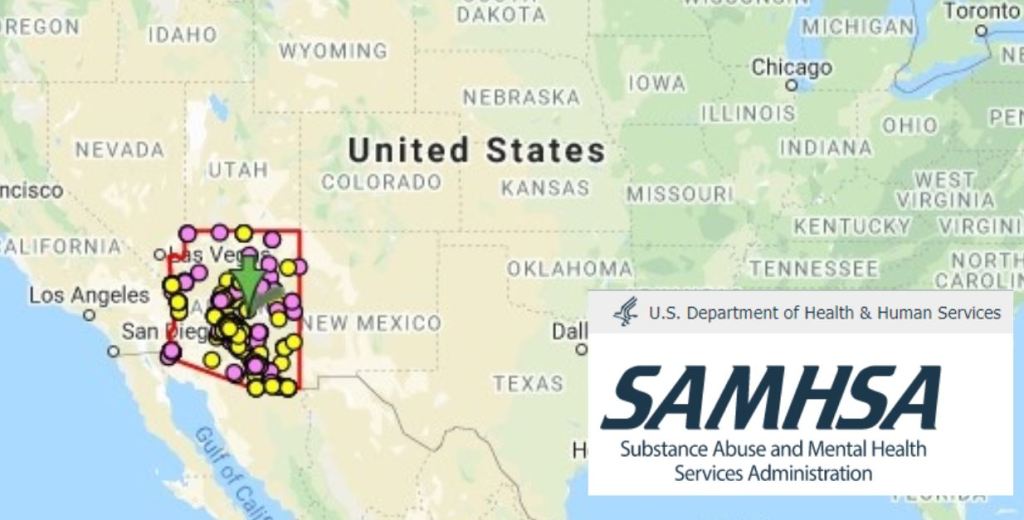
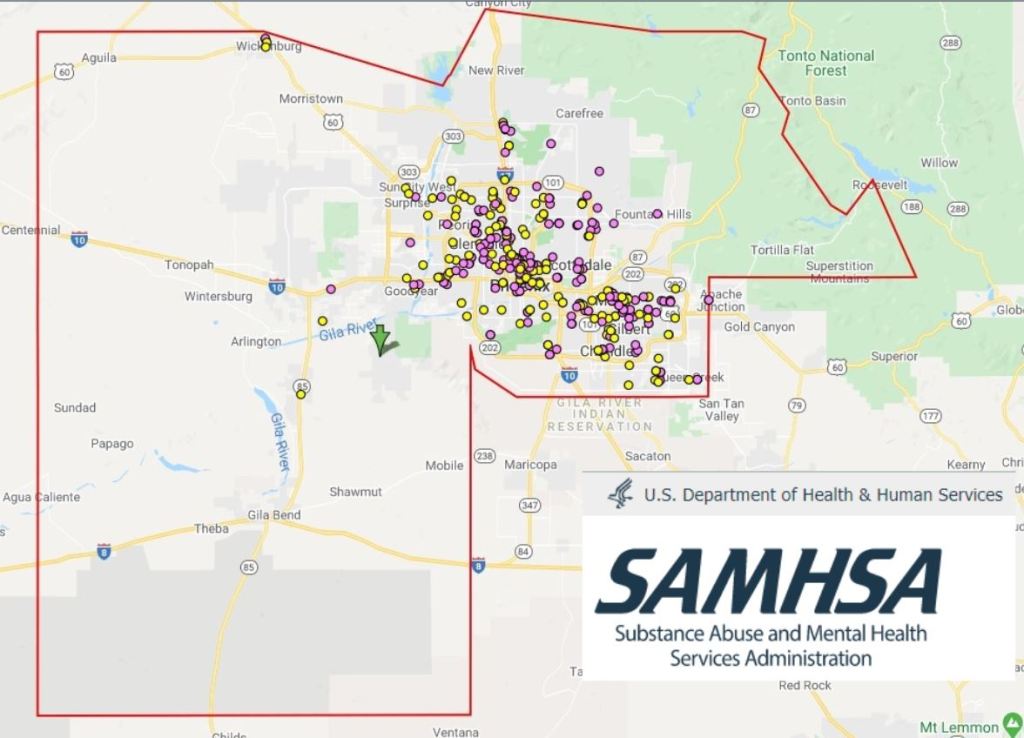
In an attempt to illuminate this complex terrain a group of interdisciplinary professionals at ASU (including this DNP scholar) is working collaboratively with local public agencies to develop a systems map of the Maricopa County mental health crisis pathways. The aim of the map development is to provide data visuals displaying frequency use nodes in this “system” and the associated costs utilization of the current, inefficient and ineffective crisis care pathway. The mapping work is developed to be a tool for policy makers improved understanding of the current system, the associated costs, as well as some of the stories from first responders and consumers for whom the system is failing. It is our hope to highlight a financial case to drive new tracks for comprehensive policy change which will drive system redesign for this critical social terrain.
I really appreciate your systems perspective on publicly funded mental health services in Arizona. As an Arizona newcomer, I often forget that AHCCCS isn’t simply an interesting name for Arizona Medicaid, but actually stands for an organization whose primary strategy is cost reduction. As we learned in DNP 713, an organization’s primary strategy exists to protect its identity (Gagliardi, 1986). Secondary strategies may exist in support of the primary strategy (Gagliardi, 1986). AHCCCS serves two masters. Although the federal government mandates state Medicaid coverage and provides parameters under which Medicaid is administered, administration itself is at the state level and is largely at the discretion of each state.
Title XIX of the Social Security Act states that all state Medicaid plans must provide eligible beneficiaries with inpatient hospital care, outpatient hospital care, laboratory services, x-rays, skilled nursing home services over the age of 21, and physician’s services, among other benefits that do not include mandates for mental illness coverage (Centers for Medicare and Medicaid Services, n.d.). From a federal perspective, Medicaid is not a cost-reduction policy and its primary strategy is to provide healthcare services to eligible low-income adults, children, pregnant women, elderly adults, and people with disabilities (Centers for Medicare and Medicaid Services, n.d.). Under the state’s direction, AHCCCS administers Medicaid to eligible Arizona residents. What remains confusing, however, is why AHCCCS bears the nominal mark of a financial primary strategy when its mission is “reaching across Arizona to provide comprehensive, quality health care to those in need” (2020). Whether AHCCCS’ primary strategy is provision of care or cost containment, providing preventive and comprehensive mental health services should fulfill these organizational imperatives.
References
AHCCCS. (2020). About the Arizona Health Care Cost Containment System (AHCCCS). https://azahcccs.gov/AHCCCS/AboutUs/index.html
Centers for Medicare and Medicaid Services. (n.d.). Access to care. https://www.medicaid.gov/medicaid/access-care/index.html
Gagliardi, P. (1986). The creation and change of organizational cultures. A conceptual framework. Organizational Studies, 7(2). https://doi.org/10.1177/01708406800700203
LikeLike